What Do You Really Know About Omegas?
SPONSORED BY SCIENCEBASED HEALTH

Laura M. Periman, MD
Laura M. Periman, MD
Evergreen Eye Center
Seattle, Washington
Laura Periman, MD is a board-certified ophthalmologist, fellowship-trained cornea and refractive surgeon and Ocular Surface Disease Expert. She knew she wanted to be a doctor since the age of 12 and always seen eyes as the key defining feature of every person. Her interests in molecular biology began with winning the Terry Spies Memorial Scholarship at the Oregon Regional Primate Research Center as an undergraduate at Willamette University in Salem, OR.
Her interests in immunopathophysiology took root during her work in Research and Development at Immunex Corporation in the Molecular Biology Department prior to attending medical school at the University of Washington in Seattle, WA. During medical school, she received the Rex and Arlene Garrison Oncology Fellowship, the Western Medical Student Research Committee Award for Excellence and was elected to the honor society, Alpha Omega Alpha. Upon graduation with honors, she also received the Georgianna Kirby Award for outstanding patient dedication and compassion.
Dr. Periman completed her Ophthalmology Residency as well as Cornea/Refractive Fellowship at the University of Washington in Seattle. She is an international lecturer on Ocular Surface Disease. She has nine peer reviewed publications, two chapters, a review article and independent study in press, and has written extensively on the topic of Ocular Surface Disease. Her unique and passionate perspective on OSD stems from her work in immunopathophysiology. She is an innovator and enthusiastic speaker who loves bridging the gap between basic science, clinical practice and patient compassion.
As Director of Dry Eye Services and Clinical Research at Evergreen Eye Center Seattle, WA she combines her clinical care passion, scientific drive and innovative creativity to provide first class Ocular Surface Disease management.
For more information on Dr. Periman, please visit her website www.dryeyemaster.com.
Omega fatty acids have long been a mainstay of dry eye treatment, and many eyecare practitioners have seen improvements in patients taking them. In this article, Dry Eye Access advisory board member, Dr. Laura Periman, explains how generalization of all omegas and lack of understanding has led to debate about their real benefit in Dry Eye Disease.
The recently published DREAM study[i] found that fish oil did not perform significantly better than the olive oil placebo in treating dry eye. Closer analysis of the study demonstrates the need to increase our understanding of formulaic differences in nutraceuticals.
Understanding Different Omegas
Omega-3 and 6 fatty acids play an integral role in our body’s ability to regulate and balance inflammation. I still remember the first study I read showing that omega-6 supplementation was helpful in Sjögren’s Syndrome patients and being shocked by information that was contradictory to what I thought I knew. This started my journey into studying and more deeply understanding the biochemistry of both omega-3s and omega-6s.
Many inflammatory cytokines (both pro-inflammatory and anti-inflammatory) are produced from omega fatty acid building blocks. The mechanism of action of NSAIDs relies on targeting the metabolism of the pro-inflammatory omega arachidonic acid. Arachidonic acid is a largely pro-inflammatory omega-6 metabolite that is over-abundant in the Western diet and is the reason omega-6s have a bad name. But, as with most things in biologic systems, there is balance and nuance and more to the story.
The omega-6 gamma-linolenic acid (GLA) is different. GLA is the only truly viable precursor to the potent anti-inflammatory PGE1, and it has been shown in multiple controlled trials to have positive effects specifically for dry eye.[ii],[iii] PGE1 is found in the tears, the lacrimal glands and the conjunctiva. Importantly, GLA has been shown to increase PGE1 levels and increase tear production in Sjögren’s Syndrome.[iv]
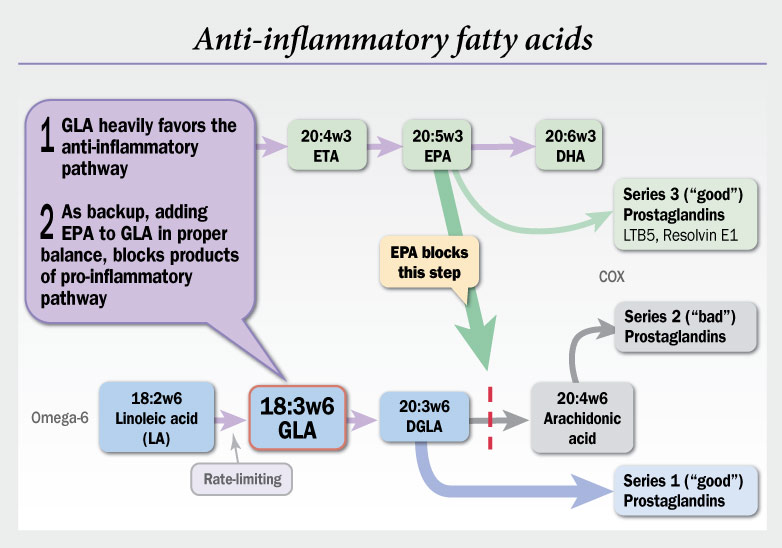
It has been shown that when GLA is combined with the proper balance of eicosapentaenoic acid (EPA) you can inhibit production of arachidonic acid[v] by the enzyme delta-5 desaturase, while stimulating production of anti-inflammatory cytokines from both GLA and EPA.[vi] By blocking the pro-inflammatory pathway, you divert the metabolic traffic flow down to one lane towards the desirable anti-inflammatory PGE1 pathway.
It is important to acknowledge that the findings of DREAM don’t apply to all omegas. How omegas are combined matters. In addition, allowing such a heterogenous study group created a more realistic pool, but also made it difficult to measure the effect of a single, non-specific intervention. As a stand-alone study and also in the context of a multitude of omega studies, the DREAM study has a lot to teach us. Perhaps we shouldn’t lump dry eye together into a few types. Perhaps dry eye is actually a dozen or more different subtypes. We do need better tests that more precisely categorize patient subtypes, rule out co-morbidities and masqueraders as well as measure disease state activity in response to therapies. We learn as much from what didn’t work as from what did. There’s no need to throw the baby out with the bath water and stop all omegas. We need dry eye studies and therapeutics to precisely describe, measure and improve a compromised lacrimal functional unit (LFU). A compromised LFU is like a mountain river ecosystem where the slope, flow, erosion, water quality, flora, fauna, etc. have somehow damaged the ecosystem’s homeostatic harmony.
Using Scientifically Proven Nutraceuticals

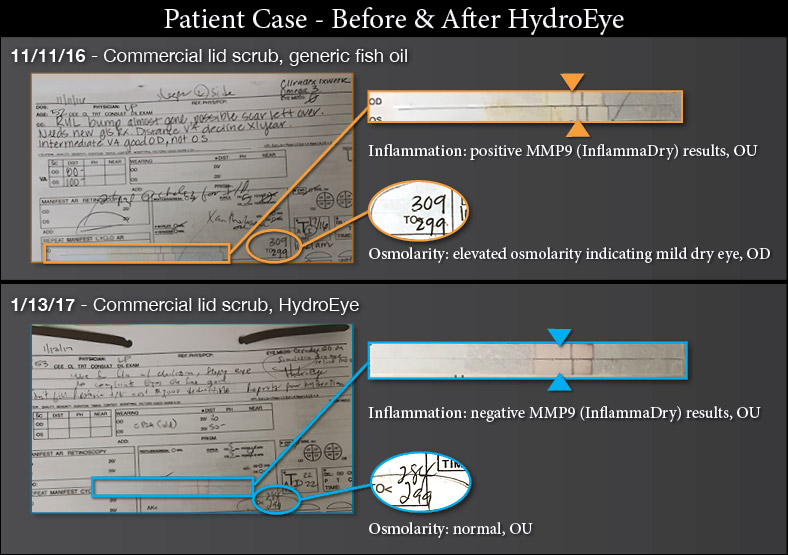
HydroEye (ScienceBased Health) is a patented oral nutritional supplement that provides a proprietary blend of GLA plus other omegas and key nutrients that work together to support all 3 tear film layers, maintaining eye moisture and providing comfort for those experiencing dry eye related to a variety of causes. A randomized, controlled, double-blind study demonstrated that consumption of HydroEye by dry eye patients significantly improved symptoms, suppressed markers of conjunctival inflammation, and maintained corneal smoothness.[vii]
Nutrition is important—you literally are what you eat and food is Foundational Medicine. Since we have the ability to repair the foundation, nutraceutical therapy as well as nutrition therapy are where I start in my practice. The anti-inflammatory omega-6, GLA, occurs in just a few plant-based oils, and is not normally obtainable at meaningful levels from our diet. Fish oil is the primary source of the omega-3s, EPA and DHA. Since our bodies cannot produce GLA, EPA or DHA directly, and since creating them through metabolism is inefficient (especially with age), nutritional supplementation fills a critical need.
I recommend HydroEye to all of my dry eye patients. Environmental, lifestyle and nutritional interventions can be especially helpful with mild, level 1 dry eye. I have personally seen excellent clinical and inflammatory burden improvements (measured by MMP9) in early Level 2 patients who took this nutritional supplement as a solo agent (patients who got too busy to start the other recommended therapies). With Level 2 patients and higher, I build upon foundational nutritional therapy by layering immunomodulators and new neurostimulation approaches.
Patients don’t want to be on prescription drugs for any longer than absolutely necessary. HydroEye improves the tear film, the lids and the Meibomian glands in a more natural way. Taking every opportunity to understand more, think deeper, and observe more carefully allows us to embrace the opportunity that science affords us. Laura Periman, MD, is the Director of Dry Eye Services and Clinical Research at Evergreen Eye Center in Seattle, WA. She has studied the immunopathophysiologic mechanisms behind dry eye disease for 29 years and believes in taking an integrated approach to treatment. She has authored many articles and has lectured domestically and internationally. To contact Dr. Periman e-mail: lauraperiman@yahoo.com.
[i] Dry Eye Assessment and Management Study Research Group. n-3 fatty acid supplementation for the treatment of dry eye disease. NEJM. April 13, 2018.
[ii] Macri A, Giuffrida S, Amico V, Lester M, Traverso CE. Effect of linoleic acid and gamma-linolenic acid on tear production, tear clearance and on the ocular surface after photorefractive keratectomy. Graefes Arch Clin Exp Ophthalmol 2003;241(7):561-6.
[iii] Kokke KH, et al. Oral omega-6 essential fatty acid treatment in contact lens associated dry eye. Contact Lens & Anterior Eye 31:141-6, 2008.
[iv] Aragona P, Bucolo C, Spinella R, et al. Systemic Omega-6 essential fatty acid treatment and PGE1 tear content in Sjogren’s syndrome patients. Investigative Ophthalmology & Visual Science 2005;46:4474-4479.
[v] Viau S, Maire MA, Bruno P, Joffre C. Eficacy of a 2-month diatary supplementation with polyunsaturated fatty acids in dry eye induced by scopolamine in a rat model. Graefes Archive of Ophthalmology 2009;247(8):1039-50.
[vi] Barham JB, et al. Addition of EPA to GLA-supplemented diets prevents serum arachidonic acid accumulation in humans. J Nutr 130: 1925-31, 2000.
[vii] Sheppard, JD, Singh R, McClellan A, et al. Long-term Supplementation With n-6 and n-3 PUFAs Improves Moderate-to-Severe Keratoconjunctivitis Sicca. Cornea. 2013;32(10):1297–1304. doi: 10.1097/ICO.0b013e318299549c.
SPONSORED BY SCIENCEBASED HEALTH
This article is adapted from an article Dr. Periman previously published in Ophthalmology Times.
