Diagnosing Inflammation of the Ocular Surface
Dry Eye Disease is a condition in which a person either does not produce enough tears or has tears of poor quality that evaporate too quickly. Tears that bathe the surface of the eye are necessary for maintaining the health of the front surface of the eye and providing clear vision. When the surface of the eye is exposed to environmental stress or is damaged, it may activate an inflammatory response that can result in the common symptoms of Dry Eye Disease.1 Over time, Dry Eye Disease may progress into a chronic condition, and can potentially damage the surface of the eye, increase the risk of eye infection, and impair vision.1-3 Dry Eye Disease is an extremely common condition that affects nearly 30 million adults in the United States.4
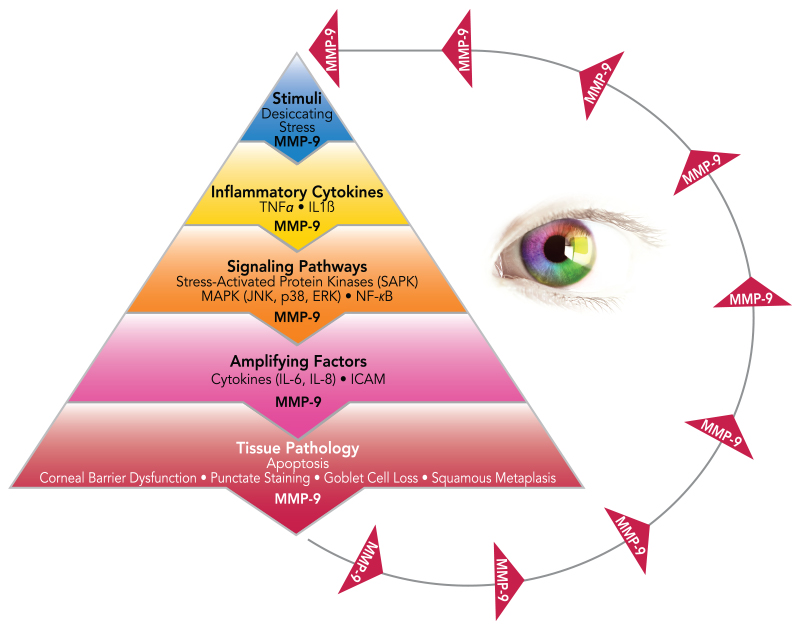
What is MMP-9?
MMP-9 is a key inflammatory marker for Dry Eye Disease and a sign of early ocular surface diseaseA number of conditions constitute ocular surface disease, including: Dry Eye syndrome, Meibomian Gland Dysfunction, blepharitis, rosacea, allergies, scarring from glaucoma medications, chemical burns,.... Matrix metalloproteinases (MMP) are proteolytic enzymes that are produced by stressed epithelial cells on the ocular surface.5,6 MMP-9 destabilizes the tear filmThe outer layer is an oil- or lipid-based layer, which helps reduce evaporation of the natural tears. and directly contributes to corneal barrier dysfunction by breaking down tight junctions and facilitating inflammatory cell migration.6
MMP-9 = Cascade of Inflammation7
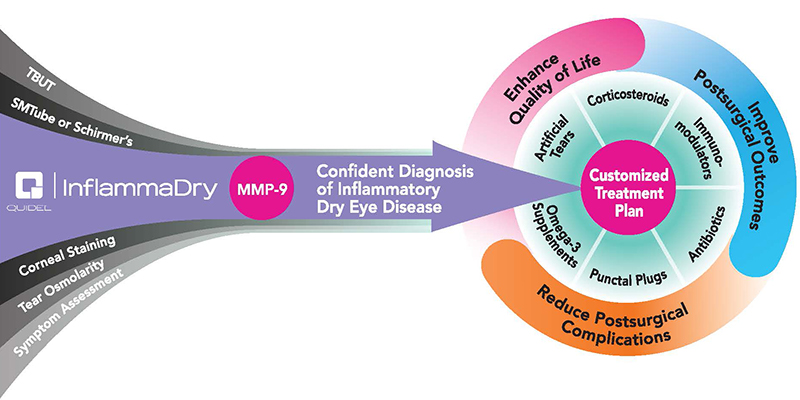
Value of MMP-9 Testing
- Single-use test without workflow impairment or ancillary equipment costs
- MMP-9 levels produce actionable events
- Avoid punctal occlusion in patients with elevated MMP-9
- Elevated MMP-9 may predict which patients will respond to anti-inflammatory therapy
- Patients who test positive can be treated with one of the following8-10: cyclosporine, lifitegrast, steroids, azithromycin, or doxycycline
- Not all dry eye patients have clinically significant inflammation
- 40% to 60% of symptomatic dry eye patients have inflammation11
- Traditional dry eye testing methods (TBUT, Schirmer’s, osmolarity) CANNOT predict which patients have inflammation12
- Identifying elevated MMP-9/inflammation helps guide Dry Eye Disease management and therapeutic decision making13
How to Diagnose Inflammation
InflammaDry® is a diagnostic test that can be performed in the eye doctor’s office to test tears for the presence of inflammation. By using the InflammaDry test to determine if there is an above normal level of inflammation on the surface of the eye, the eye doctor can determine the best and most appropriate Dry Eye treatment plan for the patient.
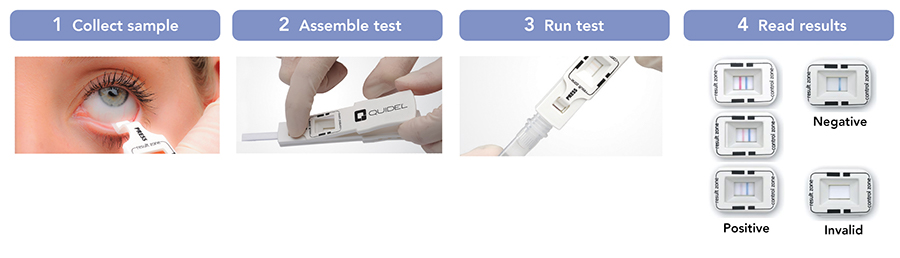
How to Perform the Test
To perform the InflammaDry test, tears are collected from the lower eyelids. Each eye requires the use of a separate test. A small, soft piece of fabric is gently dabbed along the lower eyelid to collect tears, very similar to the way a paper towel absorbs liquid from a surface. The tear collection process takes less than a minute and is not painful. Once the tear sample is collected, the test is activated, and results are provided before the patient leaves the doctor’s office. A positive InflammaDry test result indicates that there is a significant amount of inflammation on the surface of the eye.
 How to Treat Inflammation
How to Treat Inflammation
Dry Eye Disease may require an extensive treatment plan and continuous therapy. Various Dry Eye Disease treatment plans are available, based on the discretion of the doctor. Using the MMP-9 test to determine if inflammation is a factor in Dry Eye helps guide the doctor’s approach to treatment. Patients who test positive for elevated levels of MMP-9 have confirmed inflammation and may benefit from anti-inflammatory therapy. Over time, as inflammation is reduced by anti-inflammatory therapy, Dry Eye symptoms may diminish, and the overall health of the eye may improve.14i

Diagnose with Confidence
InflammaDry is the first and only, rapid, CLIA-waived, in-office test that detects elevated levels of MMP-9 using a simple 4-step process to identify patients that might otherwise be missed with other Dry Eye testing methods.4
- Accurate: 85% sensitivity, 94% specificity
- Easy to use: 4 simple steps, can be performed by a technician
- Cost effective: Single-use, disposable test
- Fast: Results in as soon as 10 minutes
- Informative: Guides appropriate therapies
Identifying elevated levels of MMP-9 facilitates better management of4:
- Patients who present with signs or symptoms of Dry Eye Disease
- Patients preparing for ocular surgery such as LASIK or cataract surgery
- Contact lens patients to better prevent and manage lens intolerance
- Glaucoma patients with significant underlying ocular surface inflammation to guide therapeutic options
References:
- Li DQ, Lokeshwar BL, Solomon A, Monroy D, Ji Z, Pflugfelder SC. Regulation of MMP-9 production by human corneal epithelial cells. Exp Eye Res. 2001;73(4):449-459.
- Corrales RM, Stern ME, De Paiva CS, Welch J, Li DQ, Pflugfelder SC. Desiccating stress stimulates expression of matrix metalloproteinases by the corneal epithelium. Invest Ophthalmol Vis Sci. 2006;47(8):3293-3302.
- Sobrin L, Liu Z, Monroy DC, et al. Regulation of MMP-9 activity in human tear fluid and corneal epithelial culture supernatant. Invest Ophthalmol Vis Sci. 2000;41(7):1703-1709.
- Chotikavanich S, de Paiva CS, Li de Q, et al. Production and activity of matrix metalloproteinase-9 on the ocular surface increase in dysfunctional tear syndrome. Invest Ophthalmol Vis Sci. 2009;50(7):3203-3209.
- Lanzini M, Curcio C, Colabelli-Gisoldi RA, et al. In vivo and impression cytology study on the effect of compatible solutes eye drops on the ocular surface epithelial cell quality in dry eye patients. Mediators Inflamm. 2015;2015:351424.
- Pflugfelder SC, Farley W, Luo L, et al. Matrix metalloproteinase-9 knockout confers resistance to corneal epithelial barrier disruption in experimental dry eye. Am J Pathol. 2005;166(1):61-71.
- Pflugfelder SC, de Paiva CS, Tong L, Luo L, Stern ME, Li DQ. Stress-activated protein kinase signaling pathways in dry eye and ocular surface disease. Ocul Surf. 2005;3(4 suppl):S154-S157.
- De Paiva CS, Corrales RM, Villarreal AL, et al. Corticosteroid and doxycycline suppress MMP-9 and inflammatory cytokine expression, MAPK activation in the corneal epithelium in experimental dry eye. Exp Eye Res. 2006;83(3):526-535.
- Gürdal C, Genç I, Saraç O, Gönül I, Takmaz T, Can I. Topical cyclosporine in thyroid orbitopathy-related dry eye: clinical findings, conjunctival epithelial apoptosis, and MMP-9 expression. Curr Eye Res. 2010;35(9):771-777.
- Li DQ, Zhou N, Zhang L, Ma P, Pflugfelder SC. Suppressive effects of azithromycin on zymosan-induced production of proinflammatory mediators by human corneal epithelial cells. Invest Ophthalmol Vis Sci. 2010;51(11):5623-5629.
- Sambursky R, Davitt WF 3rd, Friedberg M, Tauber S. Prospective, multicenter, clinical evaluation of point-of-care matrix metalloproteinase-9 test for confirming dry eye disease. Cornea. 2014;33(8):812-818.
- Lanza NL, McClellan AL, Batawi H, et al. Dry eye profiles in patients with a positive elevated surface Matrix Metalloproteinase 9 Point-of-Care Test versus negative patients. Ocul Surf. 2016;14(2):216-223.
- Kaufman HE. The practical detection of mmp-9 diagnoses ocular surface disease and may help prevent its complications. Cornea. 2013;32(2):211-216.
- Hessen M, Akpek EK. Dry eye: an inflammatory ocular disease. J Ophthalmic Vis Res. 2014;9(2):240-250.
- Schiffman RM, Walt JG, Jacobsen G, Doyle JJ, Lebovics G, Sumner W. Utility assessment among patients with dry eye disease. Ophthalmology. 2003;110(7):1412-1419.
- Shtein RM. Post-LASIK dry eye. Expert Rev Ophthalmol. 2011;6(5):575-582.
- Sambursky R, O’Brien TP. MMP-9 and the perioperative management of LASIK surgery. Curr Opin Ophthalmol. 2011;22(4):294-303.
- Marsh P, Pflugfelder SC. Topical nonpreserved methylprednisolone therapy for keratoconjunctivitis sicca in Sjögren syndrome. Ophthalmology. 1999;106(4):811-816.